

A networking app can help construct and maintain larger study cohorts
To estimate HIV incidence, conducting a prospective cohort study is recommended, however it is challenging to construct and maintain cohorts among people with HIV in China due to fear of stigma, discrimination and perceived lack of confidentiality, which has likely exacerbated the HIV epidemic.
In recent years, the extensive use of geosocial networking (GSN) apps for seeking social and sexual partners has changed the patterns of sexual behaviors in most demographic groups, including men who have sex with men (MSM). Moving from venue-directed to internet-directed networking has resulted in an increased likelihood of casual sex. However, the influence of risky sexual behaviors on HIV incidence caused by this change has not been clearly established. To better understand the role of GSN apps in influencing these behaviors we used a popular networking app to conduct our study.
How did we harness the app to estimate HIV incidence among its users?
We constructed an open cohort among MSM through an app with 40 million users worldwide, which included an HIV survey and test booking functionality. Users who wanted to be tested for HIV completed a questionnaire and booked a test via the app. Individuals who tested positive were referred to the appropriate center for disease control (CDC) for a confirmation test.
During the study period, participants who voluntarily booked two or more HIV tests via the app and completed the online survey were considered as individuals with a complete follow-up visit. Participants who had only one HIV test through the app were considered lost to follow-up in this study.
The cohort and HIV seroconversion
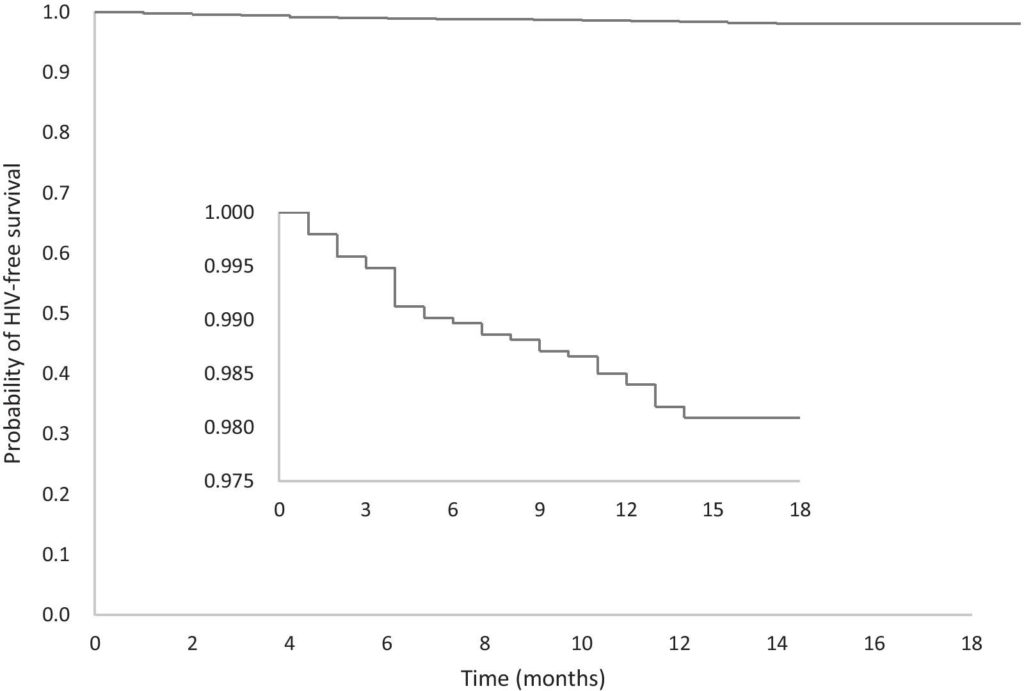
During the 18-month study period, we enrolled 6952 HIV negative men in the cohort and identified 37 HIV seroconversions among 1,937 HIV negative individuals who reported two or more episodes of HIV testing. The total person-time observed was 1,065 person-years. The estimated HIV incidence rate was 3.47 per 100 person-years (95%CI 2.37-4.57).
We found that in the six months before their last follow-up, 37.2% of participants reported two or more sexual partners, 4.5% reported having HIV-positive sex partners, while 48.3% did not know the HIV status of their sexual partners, and those who never or occasionally used condoms during anal sex accounted for 35.8%.
We found that it was not socio-demographic characteristics, but sexual behaviors that were associated with HIV seroconversion. Having more than five sexual partners as well as partners living with HIV were the dominant risk factors for seroconversion. Consistent condom use and being exclusively insertive during anal sex were protective factors against HIV seroconversion. In China, HIV incidence among users of the app was still high despite multiple interventions being implemented to reduce transmission.
In recent years, social media applications are being increasingly integrated into public health interventions. With the extensive use of dating apps, more and more interventions and health education are performed via these apps and, as a consequence, health resources are more accessible to users. In light of this, smartphone apps could potentially play an important role in promoting health and well-being beyond HIV control.