September 11, 2020
4 min read
Those in the LGBT community often face disparities in access to quality health care, leading to poorer outcomes like higher rates of STDs, researchers wrote in Annals of Family Medicine.
To reverse some of these negative health outcomes, Bruce W. Furness, MD, MPH, medical epidemiologist at the CDC, and colleagues created Transforming Primary Care for LGBT People. The 1-year intervention was tested on 441,387 patients in 123 clinical sites affiliated with 10 federally qualified health centers, or FQHCs.

According to researchers, the 1-year intervention produced significant results, including:
- a 42.9% increase in collecting patient pronoun information;
- a 276.3% jump in gathering sexual orientation and gender identity data; and
- a 300% increase in identifying LGBT patient liaisons.
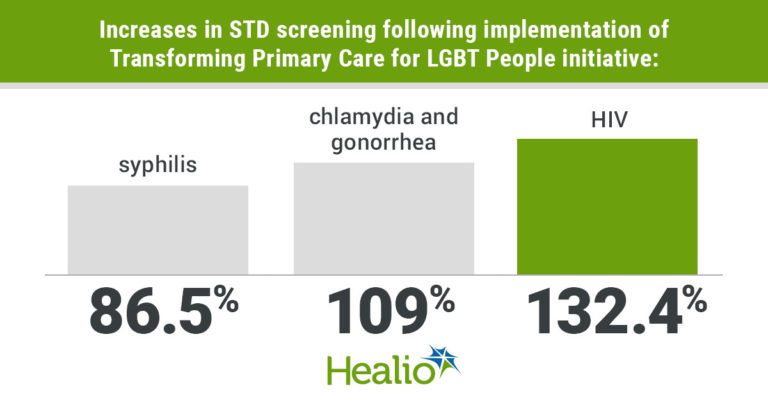
Among eight of the test sites, researchers reported increases in:
- syphilis screening by 86.5%;
- chlamydia and gonorrhea screening by 109%; and
- HIV screening by 132.4%.
Healio Primary Care spoke with Furness about the development of Transforming Primary Care for LGBT People, how to implement it and more.
Q: How did Transforming Primary Care for LGBT People come about?
A: In January 2016, CDC staff and advisers invited 12 FQHCs with a known interest in providing more LGBT-affirming care to respond to a competitive request for proposals. CDC funding allowed up to 10 FQHCs to participate. After careful review by internal and external experts, the 10 applicants that demonstrated the highest level of commitment from leadership; had the systems necessary to implement the intervention; and agreed to all intervention and evaluation activities were chosen as test sites. As the 1-year testing period went on, the intervention spread from 10 clinicians in 10 clinical sites to 431 clinicians in 79 clinical sites.
Q: What are the components of Transform i ng Primary Care for LGBT People?

Bruce W. Furness
A: The program blends two evidence-based models, the Practice Improvement Collaborative and the Project Extension for Community Health Outcomes (or Project ECHO).
The Practice Improvement Collaborative part consisted of each FQHC forming a team that included a quality improvement facilitator, a clinical champion and two or three additional staff members. Teams received monthly coaching calls with qualified project staff and accessed free resources from health centers that previously established programs to enhance the well-being of the LGBT.
Early on, the FQHC teams developed question forms and workflows to determine where, when and by whom sexual orientation and gender identity and sexual behavior questions would be asked. Staff received role-appropriate training at staff meetings and, in real time, wrote scripts for answering patient questions. Several FQHCs had LGBT patient-advisory groups provide input and feedback. Teams also worked closely with information technology staff and electronic health vendors to improve sexual orientation and gender identity and sexual risk data capture. Each team used plan-do-study-act rapid cycle tests of change with the clinical champion’s patient panel.
Gradually, teams expanded the intervention’s procedures to add additional clinicians and clinical sites within the FQHCs and helped respond when challenges arose. To increase buy-in from other FQHC staff, teams encouraged administrative leaders and governing board members to announce their support of the intervention to staff; trained all staff on LGBT health disparities and culturally affirming communication; and asked staff for feedback on proposed changes. Community engagement occurred through outreach coordinators and collaboration with local LGBT organizations. Cross-center collaborative learning took place through two in-person and three videoconference learning meetings; sharing of monthly reports of accomplishments and barriers; and contributing of questions and resources to a web-based platform.
By using Project ECHO, primary care and behavioral health clinicians could be mentored in providing high-quality, informed and affirming care to LGBT patients. Twice-monthly sessions that were facilitated by a multidisciplinary expert clinical team comprised brief didactic presentations followed by participant-led case consultation.
The ECHO sessions both enhanced and reinforced the practice improvement collaborative by focusing on STD and HIV screening, as well as other critical LGBT health topics, such as caring for youth and older adults, prescribing pre-exposure prophylaxis, screening for cervical cancer and providing gender-affirming hormone therapy.
All FQHCs received training and tools to capture quantitative data on screening and qualitative data on barriers and facilitators to implementation. Each team shared monthly data and progress reports with project staff and other teams to provoke insights and change. Senior clinical leaders at each FQHCs completed the practice assessment survey at baseline and at the end of intervention.
For each month of the intervention, FQHCs submitted de-identified and aggregated core clinical data on patients aged 13 years and older. For improved data integrity, FQHCs received coaching from project staff and resubmitted cleaned and corrected monthly data at the end of the intervention. Transcripts of mid-intervention interviews with FQHCs teams and leadership, narrative progress reports and presentations of lessons learned were also prepared and used.
Q: What are the costs associated with implementing this intervention?
A: We did not assess or measure this. But those wishing to replicate the intervention should consider the costs of patient education materials, technology support and implementation of new systems. Future interventionists may be able to create sized-down adaptations of the intervention, where small cohorts arrange peer-to-peer learning through free or low-cost videoconferencing software, which would decrease the costs for the participating center.
Q: Are there any new staff members who need to be hired to implement and maintain this intervention?
A: For those wishing to implement this intervention, there may be a need for additional hires. However, the staff members needed may already be within the organization. Each health system will need to assess the capacity of its group to decide what will be needed to both implement and maintain the intervention.
Q: What are the differences in implementing this intervention between rural and urban areas?
A: The biggest difference between rural and urban implementation was that the rural areas were less likely to realize they had sexual and gender minority clients. The rural areas were also less likely to have the experience and resources to provide these clients with appropriate care.
